Abstract
Introduction
Red blood cell (RBC) transfusion is a frequently performed medical procedure. But it is not without risk. Evidence suggests that restrictive transfusion is safe and effectively lessens the demand for blood components. Nevertheless, there exist considerable variations in transfusion practice among different centers. The hematology unit of Princess Margaret Hospital, a secondary referral center providing inpatient services for patients with various haematological malignancies and autologous stem cell transplantation, adopted a two-phase patient blood management program to reduce the demand for blood transfusions. Firstly, single-unit policy was implemented in Feb 2015 to replace the original protocol of transfusing two units of RBC in every transfusion episode. Secondly, the hemoglobin (Hb) trigger for transfusion decreased from 8g/dL to 7g/dL in asymptomatic and hemodynamically stable patients without cardiovascular disease in Aug 2016. The impact of these strategies to blood use and patient outcomes is evaluated in the present study.
Method
The study periods included 01/01/2014 - 12/31/2014 (Period A), 04/01/2015 - 03/31/2016 (Period B) and 10/01/2016 - 09/30/2017 (Period C). All patients admitted to the center during the study periods were recruited. Demographic data, RBC consumption, length of hospital stay and all-cause inpatient mortality were retrieved from the electronic medical record system. The proportions of single-unit transfusion and the mean Hb level transfusion triggers in different periods were compared with analysis of variance for continuous variables and logistic regressions for categorical variables respectively. Blood use in different periods was expressed in terms of RBC unit transfused per patient-day of hospitalization, and compared by age and sex adjusted incidence rate ratios (IRRs) obtained from zero-inflation negative binomial regression. To study the length of stay, negative binomial regression was performed to determine the age and sex adjusted IRRs for days of hospitalization in different periods. Clustering of data was further adjusted by applying robust standard errors. Generalized estimating equation for logistic regression, controlling for age, sex, days of hospitalization and number of previous admissions, was applied to compare the inpatient mortality in different periods.
Results
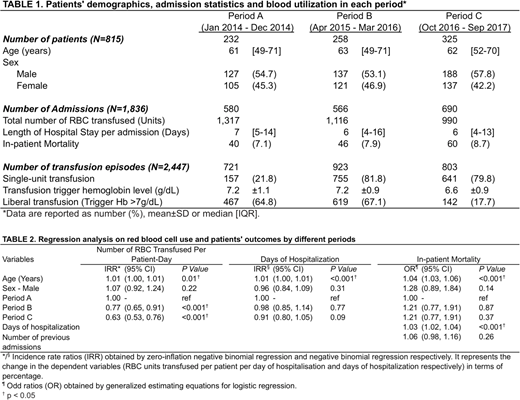
A total of 815 patients were recruited in the study, and the total number of admissions was 1,836. The number of patients in Period A was 232 (median age: 61 [IQR 49-71] years, male 54.7%) with 580 admissions, in Period B was 258 (median age: 63 [IQR 49-71] years, male 53.1%) with 566 admissions, and in Period C was 325 (median age: 62 [IQR 52-70] years, male 57.8%) with 690 admissions. The number of transfusion episodes in Periods A to C was 721, 923 and 803 respectively. The proportion of single-unit transfusion increased from 21.8% in Period A to 81.8% in Periods B (p<0.001) and 79.8% in Period C (p<0.001) respectively. The mean transfusion trigger Hb levels were 7.2±1.1 g/dL and 7.2±0.9 g/dL in Periods A and B respectively, and decreased to 6.6±0.9 in Period C (p<0.001 and <0.001). The proportion of transfusions with trigger Hb level >7g/dL decreased from 64.8% and 67.1% in Periods A and B to 17.7% in Period C (p<0.001 and <0.001) (TABLE 1).
The total number of RBC transfused in the center was 1,317 units, 1,116 units and 990 units in Periods A to C respectively. RBC transfusion rate per patient-day of hospitalization reduced by 23% in Period B (p<0.001) and by 37% in Period C (p<0.001) respectively. The median length of hospital stay [IQR] was 7 [5-14], 6 [4-16] and 6 [4-13] days in Periods A to C. The in-patient mortality rates were 7.1%, 7.9% and 8.7% in Periods A to C. There was no statistically significant difference in the length of stay and in-patient mortality between different periods (TABLE 2).
Conclusions
Our patient blood management program shows that both single-unit policy and lower Hb transfusion trigger are effective measures to reduce RBC use in hematology patients, without compromising the length of stay and inpatient mortality. Subgroup analysis could determine if restrictive transfusion strategies are applicable to all patients. Prospective studies including the occurrence of transfusion incidents and cost-effectiveness as outcome variables are useful to confirm our findings and substantiate the practicability of patient blood management.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal